Listen to the article
Three winters in a row, the same Marine Corps veteran watched his symptoms spike every November. Nightmares intensified. Anxiety got heavier.
By January, he was sleeping 12 hours a day and avoiding everyone. Then spring would arrive, and the fog would lift. He figured he was losing it until his Department of Veterans Affairs provider explained the pattern:
Winter amplifies PTSD symptoms through biology, darkness and isolation that hits veterans hard.
The Biology Behind It
Your brain needs sunlight to regulate mood and sleep. Less daylight disrupts your circadian rhythm, throwing off when your body wants to wake up or shut down. Sleep quality tanks. Energy drops. Mood follows.
Sunlight affects serotonin production. Your brain makes less of this mood-regulating neurotransmitter when you’re not getting enough light. For veterans already dealing with PTSD, this drop can push symptoms from manageable to overwhelming.
Seasonal Affective Disorder affects about 5% of the general population. Veterans with PTSD face a double hit. Seasonal depression compounds existing trauma symptoms. Intrusive memories intensify. Avoidance behavior increases. Hypervigilance spikes.
Read More: Congress Wants VA to Expand Use of AI to Flag Suicide Risk
Why Veterans Get Hit Harder
Shorter days kill motivation to go outside. Cold weather becomes another excuse to skip the gym or bail on social plans. The holidays bring financial stress and forced family interactions that trigger symptoms.
Combat veterans often deployed to extreme heat. The shift to cold can be jarring and act as a physical reminder of coming home, which itself can be a trauma trigger. Some veterans deployed during winter months, on the other hand, making the season itself a trauma anniversary.
VA research shows that light therapy consultations peak on Dec. 21 or 22, the darkest days of the year. Many veterans don’t recognize the seasonal pattern until symptoms hit crisis levels.
What the VA Offers
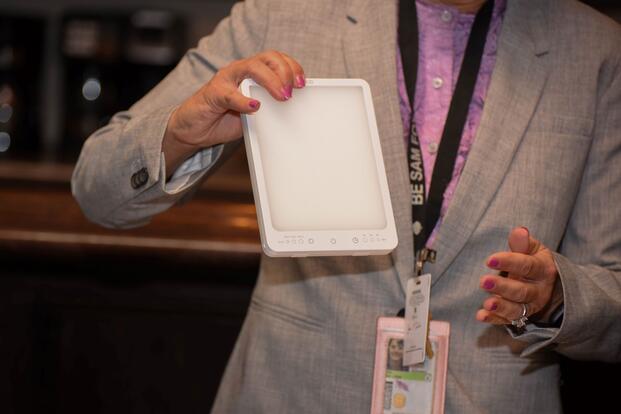
Light therapy is first-line treatment for seasonal depression and works for veterans with PTSD. The VA provides light boxes at no cost. These devices produce 10,000 lux of bright light, over 20 times brighter than typical indoor lighting. You sit in front of it for 30 minutes every morning. Most veterans experience improvement within one to two weeks.
The VA also offers cognitive behavioral therapy adapted for seasonal depression. This targets negative thoughts about winter, schedules pleasant activities despite the weather and maintains social connections during dark months.
Talk to your VA primary care provider or mental health provider about seasonal symptoms. Your provider can order a light box consult or refer you to CBT. Some VA medical centers keep light boxes available for immediate use.
Private light boxes cost between $50 and $200 if you’re not enrolled in VA care. Look for devices that produce 10,000 lux and filter out UV light. Use it first thing in the morning, not at night. Don’t stare directly at the light.
Read More: When Does the VA Cover Care at Non-VA Facilities?
What You Can Do Now
Here’s how you can start to mitigate the effects of seasonal symptoms:
- Get outside during daylight hours, even when it’s cold. A 20-minute walk in natural sunlight regulates your circadian rhythm better than any supplement.
- Exercise. It counters seasonal depression. The VA offers fitness programs, and some facilities provide free gym access. Movement increases serotonin production and improves sleep quality.
- Stay connected. Winter isolation makes PTSD worse. Veterans groups, peer support programs and regular phone calls with other veterans help maintain connections that protect against depression.
- Watch for warning signs. If your PTSD symptoms consistently worsen between November and March, document when symptoms spike so you can show your provider the seasonal connection.
- Start light therapy before the worst hits. Prevention beats crisis management.
Winter will always be darker and colder. PTSD symptoms don’t have to get worse every year.
Stay on Top of Your Veteran Benefits
Military benefits are always changing. Keep up with everything from pay to health care by subscribing to Military.com, and get access to up-to-date pay charts and more with all latest benefits delivered straight to your inbox.
Story Continues
Read the full article here

18 Comments
I appreciate that the article highlights the importance of social connections during the dark months, and I think this is an area where community-based initiatives could make a big difference.
The statistic that light therapy consultations peak on Dec. 21 or 22, the darkest days of the year, highlights the importance of addressing seasonal depression in a timely manner.
The article mentions that intrusive memories intensify during the winter months, and I think this is an area where more research is needed to understand the underlying mechanisms and develop effective treatments.
The shift from extreme heat to cold can be jarring for combat veterans, and I think this is an important factor to consider when addressing seasonal depression in this population.
I’m curious to know more about the VA’s cognitive behavioral therapy adapted for seasonal depression, and how it specifically targets negative thoughts about winter.
The article mentions that hypervigilance spikes during the winter months, and I think this is an important factor to consider when developing treatments for veterans with PTSD.
I’m supportive of the VA’s efforts to provide light therapy and cognitive behavioral therapy to veterans with PTSD, and I think these resources can make a big difference in improving symptoms and quality of life.
The fact that private light boxes can cost between $50 and $200 is a significant barrier for many veterans who are not enrolled in VA care, and I think more needs to be done to make these resources more accessible.
It’s concerning that many veterans don’t recognize the seasonal pattern of their symptoms until they hit crisis levels, and I think more needs to be done to raise awareness about this issue.
As someone who has experienced the benefits of light therapy, I can confirm that it’s effective in improving mood and reducing symptoms of seasonal depression, and I’m glad the VA offers this treatment option.
The fact that the VA provides light boxes at no cost is a significant resource for veterans, but I think more needs to be done to raise awareness about this option and make it more accessible to those who need it.
The fact that serotonin production is affected by sunlight highlights the importance of addressing the biological aspects of seasonal depression, and I think this is an area where more research is needed.
I’m excited to learn more about the VA’s efforts to expand the use of AI to flag suicide risk, and how this technology can be used to support veterans during the winter months.
I’m skeptical about the effectiveness of light therapy for veterans with PTSD, and I think more research is needed to fully understand its benefits and limitations.
Actually, studies have shown that light therapy can be a highly effective treatment for seasonal depression, and it’s often used in conjunction with other therapies.
It’s interesting that the VA provides light boxes at no cost, but I wonder if there are any other alternative treatments available for veterans who may not have access to these resources.
The fact that 5% of the general population is affected by Seasonal Affective Disorder is concerning, but it’s even more alarming that veterans with PTSD face a double hit, making their symptoms even more overwhelming.
I can attest to this, as a veteran myself, the winter months are always the toughest for me to get through.